What are UC and IBD?
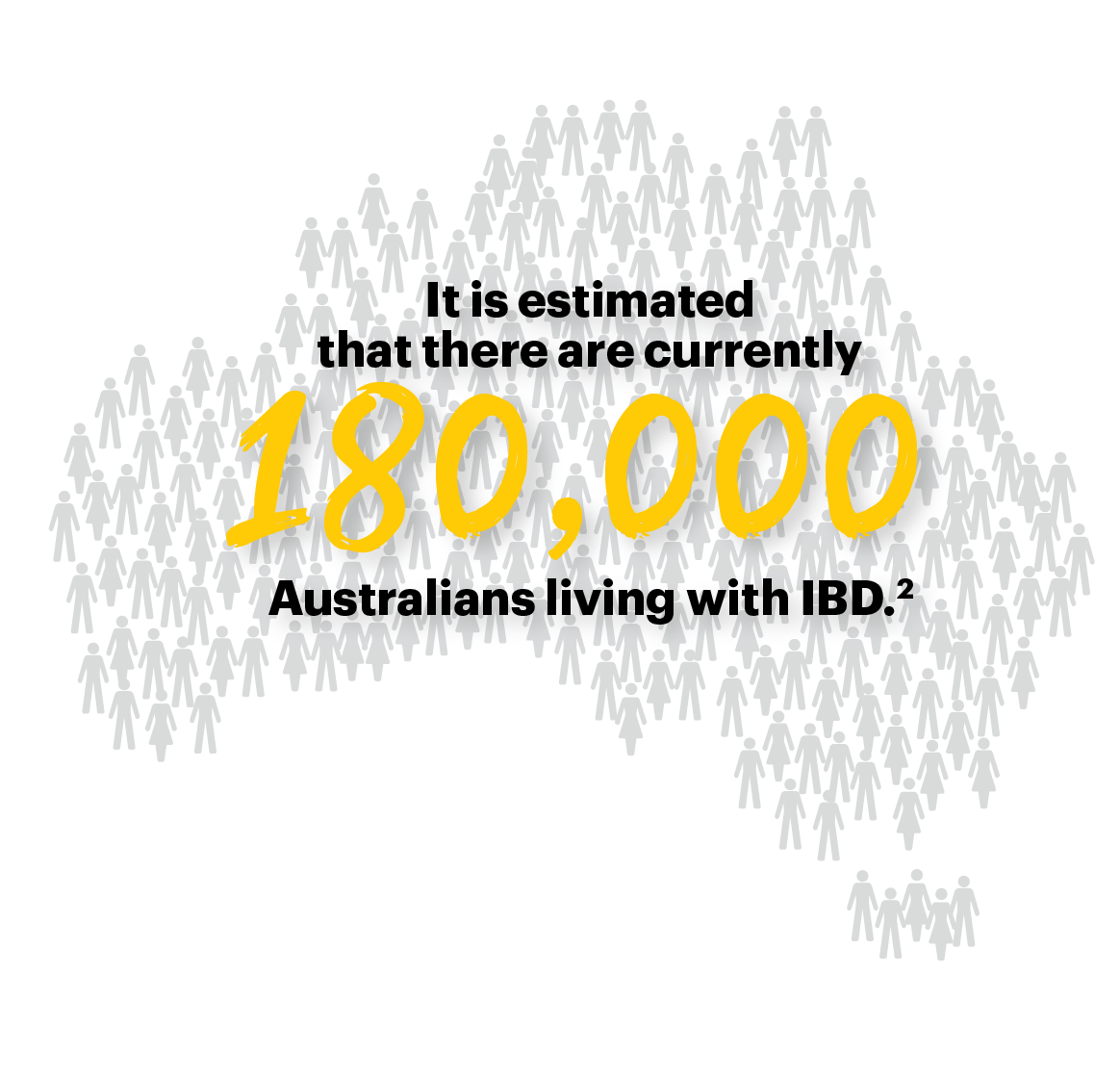
You may hear the terms UC and IBD used interchangeably, but they are not quite the same thing. IBD, or inflammatory bowel disease, describes inflammation of the bowel caused by two conditions: ulcerative colitis (UC) and Crohn’s disease (CD).1
UC causes inflammation in the inner lining of the large intestine and rectum, while CD can inflame any part of the digestive tract from the mouth to the anus and can impact the full thickness of the tract wall. Both conditions have some symptoms in common.1
The digestive tract3
This graphic is for illustrative purposes only. UC is not limited to any particular gender.
It is estimated that 5 million people around the world live with UC*4
*As of 2023.
UC can develop at any age, but usually first appears in people aged 15 to 30.1
How does UC affect people?
The symptoms of UC can vary between people and can even come and go over time depending on how inflamed the bowel is. Times when the symptoms are heightened are called flares and times when they ease are called remission. You can read more about this on our Identifying Flares and Triggers page. The main symptoms of UC can include:5,6
But these are just the obvious symptoms. Living with UC can affect people’s quality of life in many different ways; it may affect one's ability to work or impact social engagements and personal relationships. It’s also common for people living with the symptoms of UC to experience anxiety and depression as a result.7
If you are experiencing this, you are not alone and support is available. It is important to seek support if UC is affecting your quality of life and your overall health and well-being.
Visit our Communicating and Getting Support page for more information on who to seek support from.
What causes UC?
UC is an ‘autoimmune’ condition. This means the immune system mistakenly attacks the bowel tissue, and this leads to it becoming inflamed and causing the symptoms of UC.1,5,6
Although there has been a lot of research, the exact cause of autoimmune response seen in UC is not known. There seems to be some genetic influence, and UC is more common in certain ethnic groups. It’s also more common in Australia, Western Europe and America than in Asia and Africa, which may be linked with the Western lifestyle. Other lifestyle factors like diet, smoking and stress have also been linked to UC symptoms. Bacterial infection is also proposed to be a trigger for the immune response seen in UC.1,5,6
All or some of these factors may influence the development of UC, but no one factor has been shown to cause it.1,5,6
References: 1. Gastroenterological Society of Australia. Factsheet: Inflammatory Bowel Disease (IBD). Available from: gesa.org.au/public/13/files/Education & Resources/Patient Resources/IBD/16_ IBD-Crohns-Colitis_Fact-Sheet.pdf Accessed: August 2025. 2. Crohn’s and Colitis Australia. Crohn’s disease. Available from: crohnsandcolitis.org.au/about-crohns-colitis/crohns-disease Accessed: August 2025. 3. National Institute of Diabetes and Digestive and Kidney Diseases. Your Digestive System & How it Works. Available from: niddk.nih.gov/healthinformation/digestive-diseases/digestive-system-how-it-works Accessed: August 2025. 4. Berre CL et al. Lancet 2023;402(10401):571-584. 5. National Health Service. Ulcerative colitis. Available from: nhs.uk/conditions/ulcerative-colitis/ Accessed: August 2025. 6. Health direct. Ulcerative colitis. Available from: healthdirect.gov.au/ulcerative-colitis Accessed: August 2025. 7. Gastroenterological Society of Australia. Mental Health and IBD. Available from: gesa.org.au/public/13/files/Education & Resources/Patient Resources/IBD/Mental Health and IBD_v11.pdf Accessed: August 2025. AC-005092-00. AU-RNQ-250040. August 2025.